North Cumbria Integrated Care NHS Trust (NCIC) employs over 6,500 staff and provides hospital and health services to over half a million people. The Trust includes ten hospitals, and the community is spread across a broad geographical area with 51% of residents living in rural settings and over 65s making up a higher proportion of the population than the national average.
NCIC approached HBSUK for help with assessing and treating of 1200 long waiting urology patients. These patients had been waiting between 32 and 65 weeks for assessment.
The partnership with NCIC has been instrumental in reducing their waiting list size and improving patient experience with the use of Virtual Lucy. Identifying and assessing patients who have been on the waiting list for a long time has not only improved the patient experience, but has also had a significant positive impact on the delivery of care.
Nigel Meehan, HBSUK's Digital Operations Director
Patients were invited to use HBSUK’s online outpatients service, Virtual Lucy as a faster, more convenient route to getting a specialist assessment. HBSUK worked with NCIC’s Applications team to integrate Virtual Lucy with NHS Patient Administration Systems (PAS) and Electronic Health Records (EHR). The integration improved onboarding speed for patients, reduced administration within the trust and provided the timely exchange of data, whilst maintaining compliance with health data standards including HL7.
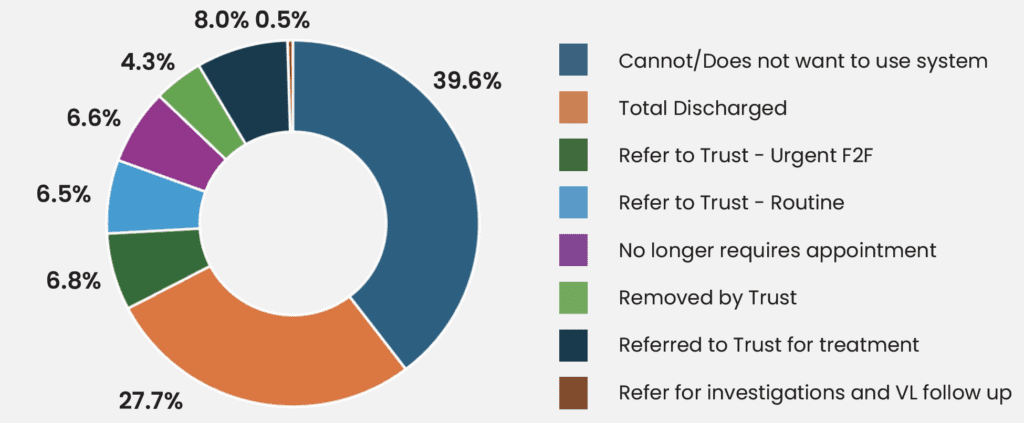
The project began in June 2024 and ran for approximately six months. 1279 long waiting urology patients were invited to complete a clinically validated online questionnaire about their condition and general health on Virtual Lucy. A combination of HBUSK and NCIC consultants reviewed each patient and provided a clinical assessment and appropriate care plan without patients needing an outpatient appointment or travelling to hospital.
Working with HBSUK helped NCIC make a significant reduction in the urology patient waiting lists.